Received: Mon 29, Jun 2020
Accepted: Tue 14, Jul 2020
Young male children are more likely than adults to sustain dog bite injuries, and up to 80% of these occur in the head and neck region [1]. Timely assessment of these injuries and appropriate decisions for surgical exploration can prevent further insult. One of the most feared complications of neurosurgical procedures in the sitting position, we present the case of a venous air embolism (VAE) in the prone position during repair of a cranial vault injury from a dog bite in a 14- month-old. Informed consent was obtained from the patient's family to publish this letter to the editor.
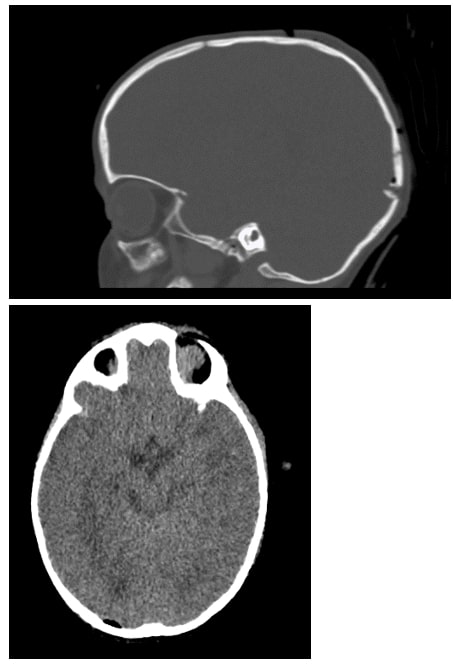
A previously healthy 14-month-old, 10 kg male presented with a dog bite injury to the scalp. At presentation, the child had injury to the parietal and occipital bones along with a left ear laceration with no evidence of hemorrhage. Brain imaging revealed three depressed, comminuted calvarial fractures of the right occipital and left temporal bones. The inferior most occipital fragment was displaced over the region of the transverse sinus. A small pneumocephalus was noted with no evidence of a midline shift or hydrocephalus (Figure 1). There was no evidence of CSF leak or rhinorrhea. Neurosurgical evaluation warranted urgent wound exploration and repair of the cranial vault injury and ear laceration.
Standard ASA monitors were placed, and the airway was secured following intravenous induction with propofol, fentanyl and rocuronium. A radial arterial line was placed in addition to a second peripheral intravenous line. The patient was flipped into the prone position and anesthesia was maintained with sevoflurane in oxygen and air. During surgical exposure, the surgeon noted substantial venous bleeding and the patient was placed in reverse-trendelenburg position. Packed red blood cells were transfused at 20 ml/kg. As the surgeon was manipulating bone overlying the right transverse sinus, hypotension was noted with BP 54/32, along with an abrupt drop in end-tidal CO2 and loss of the pulse oximeter tracing. Shortly thereafter, the patient became bradycardic (HR 45-50).
A presumptive diagnosis of an intraoperative venous air embolism was made. Epinephrine 100 micrograms was administered, and the bed was placed in trendelenburg position. The surgeon was asked to irrigate the field with warm saline. The heart rate returned to the mid-120s with return of end-tidal CO2 and the patient’s blood pressure recovered over the next several minutes to ~ 95/55 mmHg. The procedure concluded uneventfully, and the patient remained hemodynamically stable. The patient was transferred to the Pediatric ICU with the endotracheal tube in place.
Venous air emboli are a well-known and often clinically asymptomatic complication of neurosurgical procedures where the operative site is above the level of the heart [2]. In our patient, reverse trendelenburg positioning in a hypovolemic patient likely led to the entrainment of air into the dural venous sinuses leading to hemodynamic instability. The sudden loss of end-tidal CO2 associated with acute hypotension and bradycardia is strongly suggestive of a venous air embolism. A significant volume of air in the venous system may cause right ventricular outflow tract (RVOT) obstruction, while air in the pulmonary vascular bed can induce capillary permeability changes, pulmonary hypertension and edema [3].
A precordial doppler is the most sensitive and least invasive modality capable of detecting as little as 0.25 mL of air. Transesophageal echocardiogram is also highly sensitive and capable of detecting even minute amounts of intravascular air but is invasive and requires an anesthesiologist who is trained in its use. A high index of clinical suspicion for VAE is necessary for appropriate diagnosis and treatment as decreases in end-tidal CO2 and diminished pulse oximetry or arterial wave-form tracings are non-specific and occur with other low cardiac output conditions [4].
If a VAE is suspected, it is recommended to flood the field with irrigation, utilize bone wax to decrease venous bleeding, place the patient in trendelenburg position to remove air from the RVOT, and initiate jugular venous compression. A central venous catheter allows air to be aspirated directly from the right atrium. Inotropes can be utilized in a hypotensive patient to augment myocardial contractility, reduce RVOT obstruction and allow passage of emboli into the pulmonary circulation. Communication between the anesthesiologist and surgeon is integral to the diagnosis and successful management of a VAE.
REFERENCES
- Weiss HB, Friedman DI, Coben JH “Incidence of dog bite injuries treated in emergency departments.” JAMA, vol. 279, no. 1, pp. 51-53, 1998. View at: Publisher Site | PubMed
- Mirski MA, Lele AV, Fitzsimmons L, et al. “Diagnosis and treatment of vascular air embolism.” Anesthesiology, vol. 106, no. 1, pp. 164-177, 2007. View at: Publisher Site | PubMed
- Tobias JD, Johnson JO, Jimenez DF, et al. “Venous air embolism during endoscopic strip craniectomy for repair of craniosynostosis in infants.” Anesthesiology, vol. 95, no. 2, pp. 340-342, 2001. View at: Publisher Site | PubMed
- Spence NZ, Faloba K, Sonabend AM, et al. “Venous Air Embolus During Scalp Incision.” J Clin Neurosci, vol. 28, pp. 170-171, 2016. View at: Publisher Site | PubMed
