Received: Thu 16, Jul 2020
Accepted: Mon 02, Nov 2020
Abstract
Background: Synchronised cardioversion (SC) is used to terminate tachycardic arrhythmia by applying electric current to the thorax. SC is synchronised to the R wave of the cardiac cycle and ventricular tachycardia (VT) or ventricular fibrillation (VF) can occur if an electrical shock is provided in a non-synchronised way.
Case Presentation: Here we present a case of a 66-year-old man who had elective cardioversion for atrial fibrillation worsened by severe left ventricular impairment. A manual defibrillator was used for the cardioversion, which, after the first synchronised shock, reverted to defibrillator mode. An unsynchronised shock was administered and induced VT, which was reverted to sinus rhythm with a defibrillation shock.
Conclusion: When using manual defibrillator for SC, the machine needs to be set to a synchronised mode. The synchronisation to the R wave needs to be checked before every shock.
1. Background
Supraventricular Tachycardia (SVT) is an umbrella term used for any tachycardic rhythm (faster than 100 beats per minute) that does not originate in the ventricles. This includes sinus tachycardia, junctional tachycardia, re-entrant tachycardias, multiple atrial tachycardias (MAT), atrial fibrillation (AF), and atrial flutter. The electrocardiography (ECG) findings during SVT show rapid, narrow (less than 0.12 seconds) QRS complexes. Although various supraventricular rhythms can cause SVT, clinically, they are treated using the same approach.
Synchronised cardioversion (SC) is a procedure where the transthoracic electrical current is applied to the anterior chest to terminate tachycardic arrhythmia. It is performed on patients that still have a pulse but may be hemodynamically unstable or have significant co-morbidities. Unlike defibrillation, which can be applied at any point in the cardiac cycle, SC is synchronised to the R wave of the cardiac cycle. If an electrical shock is provided during the other part of the cycle, especially the relative refractory period corresponding to the second half of the T wave, it can induce ventricular tachycardia (VT) or ventricular fibrillation (VF) (the so-called “R-on-T phenomenon”). This could result in a patient who originally had a pulse being put into cardiac arrest. The other difference between SC and defibrillation is the amount of energy needed to convert the rhythm. The recommended energy levels used to perform SC vary from 50 to 200 joules, while defibrillation requires 150-200 joules [1].
To avoid inducing cardiac arrest during SC, the defibrillator is placed into the “synchronise” mode. A synchronising marker will appear above each QRS complex, indicating that the synchronise feature is active. The operator then selects the appropriate energy level (less for SC) and presses the discharge button. The defibrillator then releases the shock at the next R-wave, avoiding the R-on-T phenomenon. VT, VF and pulseless electrical activity (PEA) are the most common causes of sudden cardiac arrest in adults. VT can occur in the presence of a pulse; often, it is the precursor to VF. VT is characterized by rapid, wide (greater than 0.12 seconds) QRS complexes.
2. Case Presentation
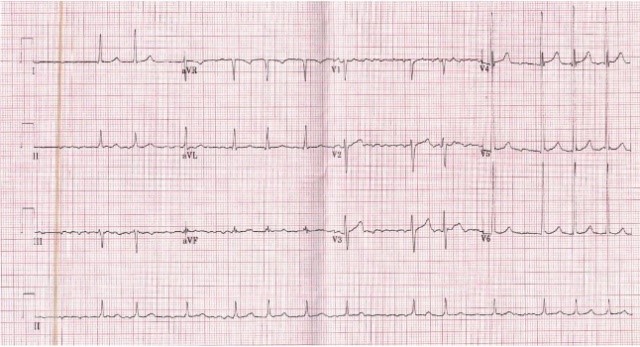
A 66-year-old man presented for an elective cardioversion for his previously diagnosed atrial fibrillation (AF) (Figure 1). Two months prior to this planned SC, the patient had an echocardiography, which showed severe left ventricular impairment with moderate mitral regurgitation and atrial dilatation. He also had significant diastolic dysfunction and elevated left-sided filling pressures. Based on those findings, the SC was planned.

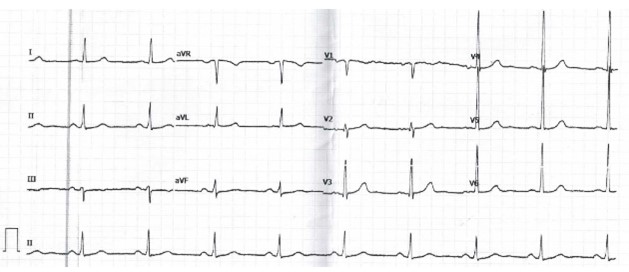
A manual defibrillator was used for the cardioversion. A junior doctor was performing the procedure supervised by the middle-grade doctor. Pt was anticoagulated in the preceding weeks, and deep sedation was achieved prior to the procedure using intravenous injection of a slow bolus dose of propofol (0.5 mg/kg). Upon the first synchronised 120 joules discharge, patient was still in AF. The shock was then repeated at 150 joules without notice of the synchronisation setting. Upon the second shock, the patient has developed VT (Figure 2). A 200 joules defibrillation shock was rapidly administered, and the patient reverted to the sinus rhythm in which he remained until discharge (Figure 3). The patient did not suffer any respiratory or cardiovascular compromise. The manual defibrillator machine was sent to the manufacturer for investigation, and the outcome suggested that it was not synchronised at the time of the second shock.
3. Discussion
SC has several known potential complications. Sedation can cause hypoxia or hypoventilation. Several cardiac complications may occur, including bradycardia, asystole or Takotsubo cardiomyopathy. These occur more often in patients with advanced age, long-standing AF or using high doses of beta- or calcium blockers and antiarrhythmic agents [2]. Other complications include hypotension and pulmonary oedema. Superficial or partial-thickness burns may occur from the electric shock. Some of these complications appear critical, however in a study of 193 patients with normal and reduced left ventricular function, troponin I measurements after cardioversion were not elevated, suggesting a lack of myocyte injury [3]. In general, SC is considered a safe and effective method of restoring sinus rhythm, if performed under the care of well-trained personnel.
Our case highlights another important side effect that may occur during SC: the potential of SC to cause VT/VF if not properly synchronised. This is particularly pertinent to manual defibrillators that need to be set to a synchronised mode after every shock to ensure they are not in defibrillation mode. Avoiding the R-on-T phenomenon is crucial for a successful and safe performing of SC.
4. Conclusion
When using manual defibrillator for SC, the machine needs to be set to a synchronised mode. The synchronisation to the R wave needs to be checked before every shock.
Author Contributions
DP: Reported the case, collected background information, wrote and edited the manuscript; TA: Managed the patient and reported the case; HA: Collected background information, edited the manuscript.
Conflicts of Interest
None.
Funding
None.
Ethical Approval
Not required.
Consent
Consent was obtained from patient.
REFERENCES
- Goyal A, Sciammarella JC, Chhabra L, et al. “Synchronized Electrical Cardioversion.” StatPearls, 2020. View at: PubMed
- Siegfried JS, Bhusri S, Guttenplan N, et al. “Takotsubo cardiomyopathy as a sequela of elective direct-current cardioversion for atrial fibrillation.” Tex Heart Inst J, vol. 41, no. 2, pp. 184-187, 2014. View at: Publisher Site | PubMed
- Cemin R, Rauhe W, Marini M, et al. “Serum troponin I level after external electrical direct current synchronized cardioversion in patients with normal or reduced ejection fraction: no evidence of myocytes injury.” Clin Cardiol, vol. 28, no. 10, pp. 467-470, 2005. View at: Publisher Site | PubMed
