Schizophrenia is a chronic psychotic illness that begins in late adolescence and lasts a lifetime. The disorder is characterized by disturbances in thought, perception, emotion and behaviour. It is a mental disorder where the person faces difficulty in distinguishing what is real and what is not. Although effective antipsychotic medications are available, patients and their families often find it hard to access adequate care.
A Closer Look at Schizophrenia
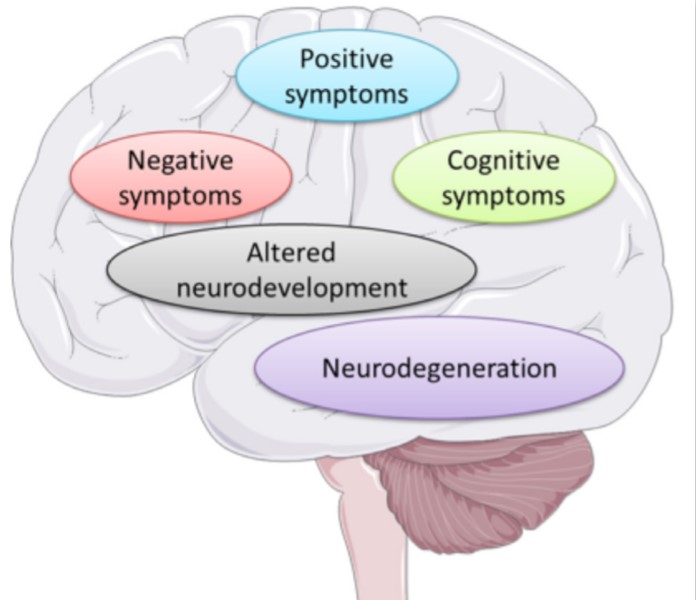
There is a misconception that schizophrenia is a split personality disorder but there is no connection between them. Instead, schizophrenia is a thought disorder that splits the patient’s thoughts, resulting in the confusion between reality and fantasy. People with schizophrenia typically experience different symptoms like hallucinations, delusions, incoherence of speech and impaired cognitive ability. Social withdrawal typically precedes a person’s first psychotic episode; however, some individuals may exhibit no symptoms at all. The regions of the brain that control and coordinate thinking, perceptions and behaviours fail to function properly, thus making it difficult for people to filter and process information. Hence, people experience mixed information that comes into their senses. Symptoms fall into three major categories: i) Positive symptoms which include hallucinations, delusions, hearing or seeing imaginary things. ii) Negative symptoms include lack of pleasure, trouble with speech, inability to express emotion. iii) Disorganized symptoms include disordered thinking and speech, trouble with logical thinking and sometimes bizarre behaviour or abnormal movements.
What Causes Schizophrenia?
Although genetics, environmental factors, neurological involvement all contribute to causing schizophrenia, the exact cause is still unclear.
Genetic Factors
Schizophrenia is mostly inherited. If there is a history of schizophrenia in a family, the offspring are at high risk of developing schizophrenia at a certain point of time. Scientists have discovered specific genes and genetic mutations that are associated with this disorder.
Environmental Factors
Environmental factors are one of the most critical risk factors for schizophrenia. Exposure to famine, radiation, prenatal events like toxemia and hypoxia at birth, obstetric complications, central nervous system infections and psychosocial stress are significant risk factors for schizophrenia. The use of marijuana and other forms of drugs increases the future risk of schizophrenia fourfold.
Neurological Factors
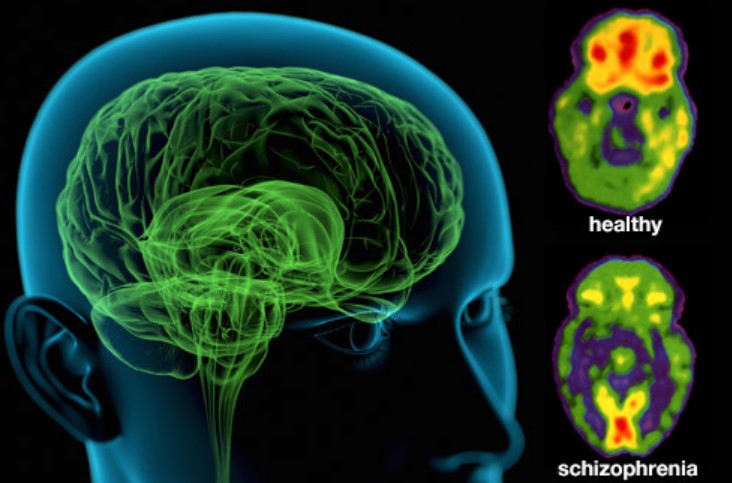
Dopamine Theory
Dopamine modulates brain functions by regulating motor control. Impairments of such brain functions may result in psychosis. For more than 40 years, we have known that excessive dopamine transmission in the brain's mesolimbic system plays a crucial role in schizophrenia. Antipsychotics mainly target dopamine D2 receptors. The hyperactive state of dopamine in mesolimbic areas produces positive symptoms, whereas insufficient dopamine transmission may underlie cognitive deficits and negative symptoms of schizophrenia. The advancement of novel antipsychotics largely depends on this dopamine theory of schizophrenia as it was observed that positive symptoms can be treated with dopamine receptor antagonists. Antipsychotics bind to the dopamine receptor and lessen the activation of dopamine neurons which reduce brain-wide dopamine release. However, these are relatively ineffective in treating negative symptoms and cognitive deficits of schizophrenia.
Glutamate Theory
Over many years, the dopamine hypothesis has been a dominant theory of schizophrenia development. However, new research suggests that glutamate might be a key to understanding schizophrenia as glutamate contributes to brain development, communicates between different areas of the brain and plays a vital role in long-term potentiation, a process by which new information or skills are retained for later use. Disruption in the glutamatergic neurotransmission may influence synaptic plasticity and cortical microcircuitry. Antipsychotics may influence glutamate transmission by affecting the release of glutamate or by interacting with glutamatergic receptors.
Treatment
Currently, there is no cure for schizophrenia but it can be managed by therapies. Scientists are unraveling the causes of the disease by studying genetics, conducting behavioural research, and using advanced imaging to observe brain’s structure and function. Treatment guidelines recommend a combined approach with pharmacologic agents and psychological interventions to prevent relapse of psychosis. Antipsychotics are the primary treatment of schizophrenia. Currently available antipsychotics mainly target positive symptoms by triggering dopamine D2 receptors but negative and cognitive symptoms are still incurable. Clozapine is known to be the most effective antipsychotic but it has short and long-term side-effects. In fact, antipsychotic medications come with some troubling side-effects, whereas non-pharmacological approaches such as therapy and psychosocial interventions may reduce relapses and help people cope with stress. Although patients can increase adaptive functioning through available pharmacological and non-pharmacological treatment options, hopefully, future research findings will address gaps in treatment and eventually will come up with a cure for schizophrenia.