Received: Thu 15, Oct 2020
Accepted: Mon 02, Nov 2020
Abstract
Hepatocellular adenoma is a rare, benign liver neoplasm. Hepatocellular adenomas carry a risk of malignant transformation and spontaneous bleeding, and giant hepatic adenomas can cause additional morbidity by compressing important adjacent structures. Surgical resection is recommended for large adenomas and is curative. We report a case of a 31-year old Hispanic male with a giant 35cm hepatocellular adenoma causing right lung compression/collapse, pulmonary hypertension, mesenteric ischemia, refractory hypertension, and cerebrovascular accident (CVA) due to renal vein compression. Exploratory laparotomy, median sternotomy, left lobectomy, cholecystectomy and hepatico-jejunostomy were performed. The giant adenoma was successfully removed with the resolution of all associated medical problems and a full recovery. Massive liver lesions can be resected safely with adequate exposure and may require median sternotomy. Multiple medical problems due to compression can be completely reversed with resection of these benign but giant lesions. Enucleation of giant adenomas is an acceptable form of treatment for lesions causing multiple symptoms due to compression and leads to a cure in most cases.
1. Introduction
Hepatocellular adenoma is a rare, benign liver neoplasm. Its incidence is projected to be 0.1 per 100,000 in non-oral contraceptive users and 3 to 4 per 100,000 in long-term oral contraceptive users [1-4]. Hepatocellular adenoma can also occur spontaneously or in association with underlying metabolic diseases such as type 1 glycogen storage disorder, diabetes mellitus or iron overload [4, 5]. The risk of malignant transformation is about 10% [4, 6, 7]. The risk is higher in men and in patients with large adenomas [4]. The risk of spontaneous bleeding is 20-40% and is increased when the tumor is greater than 5cm in diameter [8]. Surgical resection is curative and also prevents bleeding or malignant transformation. Small adenomas less than 4cm can be treated non-operatively by stopping oral contraceptive pills and monitoring with serial imaging studies [4]. Giant hepatic adenomas can cause morbidity by compression of adjacent organs, bleeding from spontaneous rupture, or malignant transformation [4].
2. Case Description
This patient is a 31-year-old Hispanic male with a giant 35cm hepatocellular adenoma involving the left lobe and the right anterior segment of the liver. He complained of fatigue, dyspnea, and early satiety requiring the use of medical marijuana. His past medical history was significant for severe hypertension, intraventricular hemorrhage without sequela, hypercholesterolemia, and anemia. The hypertension was difficult to control, requiring four antihypertensive medications. There was no history of steroid use, iron overload, glycogen storage disease, or diabetes mellitus.
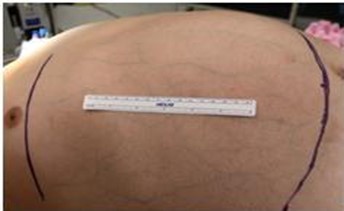
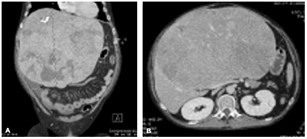
Clinically the patient appeared non-toxic but clearly cachectic with temporal wasting. He had decreased breath sounds on the right. His abdomen was soft and distended with a large palpable mass that extended from the xiphoid process down to below the umbilicus and into the left upper quadrant (Figure 1). There was evidence of portal hypertension with dilated veins on the abdominal wall. There was no associated abdominal pain, fluid shift, or hepatojugular venous reflux. Laboratory values were within normal limits. A computed tomography scan showed a 35 x 28 x 16.5cm mass arising from the liver and extending inferiorly to the level of the L4-L5 interspace (Figure 2A). The main portal vein and inferior vena cava were compressed but patent (Figure 2B). The mass was inhomogeneous and hypoenhancing compared to normal liver parenchyma with some areas of calcifications. Upper endoscopy did not demonstrate any evidence of esophageal or gastric varices.
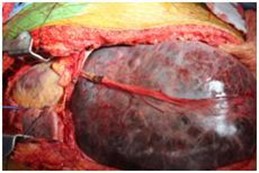
The patient underwent exploratory laparotomy, median sternotomy, left lobectomy and Roux-en-Y hepaticojejunostomy. A midline laparotomy was performed (Figure 3). The right posterior liver segment did not show any evidence of cirrhosis or mass. A median sternotomy was then performed to gain access to the intrapericardial portion of the inferior vena cava (IVC). The hilum was dissected to isolate and ligate the left sided structures. Prior to transection of parenchyma, the patient became very acidotic and hyperkalemic, requiring intra-operative dialysis presumably related to ischemia of the massive adenoma. The adenoma was enucleated off of hepatic parenchyma towards the right hepatic vein. Intermittently a Pringle maneuver was performed along with total vascular isolation. The patient became coagulopathic after the transection of the liver parenchyma. Ultimately each bleeding site was sutured with 6-0 PDS suture. A crossed over right posterior duct system was identified during the transection. Roux-en-Y hepaticojejunostomy was performed to the right anterior and right posterior ducts, entering separately.
The patient was extubated on postoperative day two. Liver function tests normalized quickly. The postoperative course was complicated by a bile leak causing a refractory right sided pleural effusion. The bile leak required the placement of a pigtail drain and antibiotics. He was discharged home after four weeks. The final pathology report confirmed the diagnosis of hepatocellular adenoma with atypical features including hepatocellular rosette formation, focally thickened liver cell plates, and focal hepatocellular pleomorphism. Special stains for reticulin and immunohistochemistry for glypican-3 supported the diagnosis. Surgical margins were negative.
3. Discussion
Hepatocellular adenomas are encapsulated benign neoplasms, which have a propensity to bleed. They very rarely undergo malignant transformation [4-6, 8]. Large adenomas have a higher risk of bleeding and malignant transformation. Adenomas are composed mostly of hepatocytes with variable numbers of Kupffer cells and no biliary ducts [4]. The diagnosis is based on history and imaging studies. Computed tomography and magnetic resonance imaging scan are the best imaging modalities. Small adenomas less than 4cm can be treated non-operatively with discontinuation of oral contraceptives and follow-up with serial imaging. Large tumors should be treated surgically owing to the risk of hemorrhage and malignant transformation.
Giant adenomas should be resected, especially if there is no evidence of malignant transformation. Adequate exposure is required to ensure resectability and allow preservation of remaining liver segments. Median sternotomy was necessary in this case in order to manipulate the tumor upward and out of the abdomen, allowing access to the hilum and control of outflow vessels. Median sternotomy can be helpful to improve access to the suprahepatic vena cava, allow tumor manipulation to access the hilum of the liver, and provide access for emergent veno-veno bypass [9].
Multiple medical problems were completely reversed with resection of the lesion. This patient was suffering from severe refractory hypertension due to compression of the renal vessels and the vena cava, also leading to CVA and headaches. The hypertension resolved immediately postoperatively, and the patient has not required antihypertensive medications at one year of follow-up. His dyspnea on exertion and fatigue disappeared completely, and he no longer has early satiety, which led to complete resolution of his malnutrition and need for appetite stimulants. At one year of follow-up there was no evidence of disease recurrence.
4. Conclusion
Massive liver lesions can be resected safely with adequate exposure and may require median sternotomy. Multiple medical problems due to compression can be completely reversed with resection of these benign but giant lesions. Enucleation of giant adenomas is an acceptable form of treatment for lesions causing multiple symptoms due to compression and leads to a cure in most cases.
Conflicts of Interest
The authors do not have any financial relationship with any company. All the authors are employees of USC University Hospital.
Funding
None.
Data Availability
The authors have full control of primary data and agree to allow the journal to review the data if requested.
REFERENCES
- Rooks JB, Ory HW, Ishak KG, et al. “Epidemiology of hepatocellular adenoma. The role of oral contraceptive use.” JAMA, vol. 242, no. 7, pp. 644-648, 1979. View at: PubMed
- Sherlock S “Hepatic adenomas and oral contraceptives.” Gut, vol. 16, no. 9, pp. 753-756, 1975. View at: Publisher Site | PubMed
- Baum JK, Bookstein JJ, Holtz F, et al. “Possible association between benign hepatomas and oral contraceptives.” Lancet, vol. 2, no. 7835, pp. 926-929, 1973. View at: Publisher Site | PubMed
- Belghiti J, Vilgrain V, Paradis V “Benign liver lesions. In Surgery of the Liver, Biliary tract and Pancreas, 4th ed.” Philadelphia, vol. 2, pp. 1131-1151, 2006.
- Labrune P, Trioche P, Duvaltier I, et al. “Hepatocellular adenomas in glycogen storage disease type I and III: a series of 43 patients and review of the literature.” J Pediatr Gastroenterol Nutr, vol. 24, no. 3, pp. 276-279, 1997. View at: Publisher Site | PubMed
- Kerlin P, Davis GL, McGill DB, et al. “Hepatic adenoma and focal nodular hyperplasia: clinical, pathologic, and radiologic features.” Gastroenterology, vol. 84, no. 5, pp. 994-1002, 1983. View at: PubMed
- Foster JH, Berman MM “The malignant transformation of liver cell adenomas.” Arch Surg, vol. 129, no. 7, pp. 712-717, 1994. View at: Publisher Site | PubMed
- Barthelemes L, Tait IS. “Liver cell adenomas and liver cell adenomatosis.” HPB (Oxford), vol. 7, no. 3, pp. 186-196, 2005. View at: Publisher Site | PubMed
- Nagano Y, Togo S, Tanaka K, et al. “The role of median sternotomy in resections for large hepatocellular carcinomas.” Surgery, vol. 137, no. 1, pp. 104-108, 2005. View at: Publisher Site | PubMed
