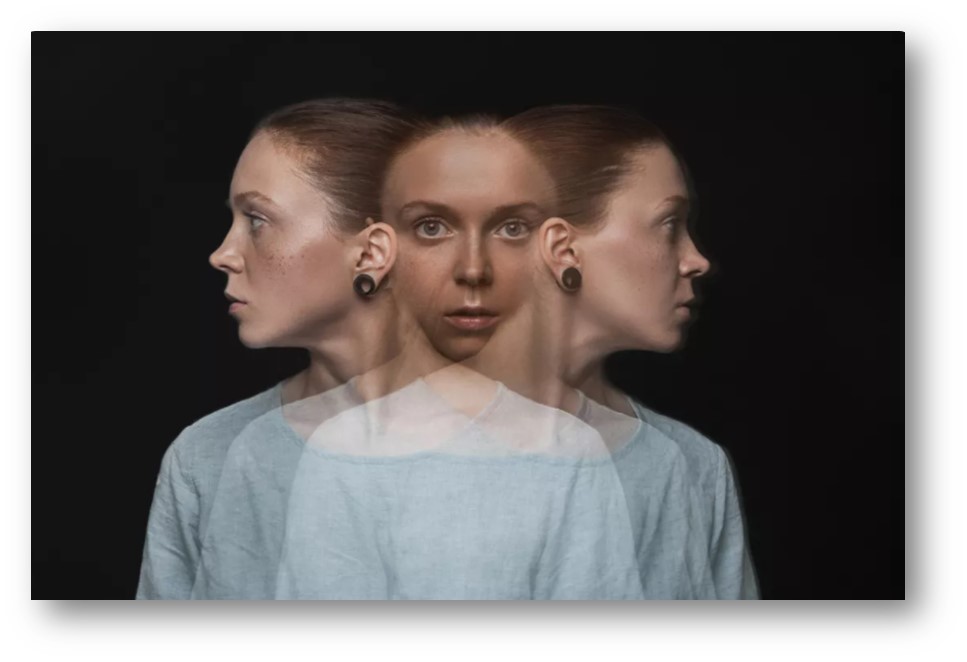
Seeing a loved one suffering from Dissociative Identity Disorder (DID) can be painful. It may be difficult keeping track of all the personalities they experience. Often, persons with DID cannot understand which of the alters is dominant at a particular time. Integration can bring about significant changes in a personality as different alters grow and change dramatically.
Dissociative identity disorder (DID) is a complex, post-traumatic developmental disorder for which we now have an authoritative research base after four decades of research. However, a number of misconceptualizations and myths about the disorder remain, compromising both patient care and research. DID is a complex psychiatric condition characterized by the development of one or more alternate personalities that works without the awareness of the person's usual personality. It is caused due to severe trauma during early childhood which usually involves extreme, repetitive physical, sexual or emotional abuse. DID is an acute form of dissociation that causes a disruption in a person's thoughts, memories, perceptions, actions, or sense of identity.
DID is a rare condition that affects around 1% of the community population. A person while suffering from DID experiences the presence of two or more distinct identities or personality states. Among these, at least two personalities recurrently take control of the person’s behaviour. The person often becomes forgetful about his/her actions when he/she is into his/her altered personality. Dissociative disorders cause disruptions or breakdowns of memory, consciousness or awareness, identity and perception. Dissociation is thought of as a coping mechanism that a person uses to disconnect from a stressful or traumatic situation. It breaks all the connection between the person and the outside world to protect himself/herself from the traumatic consequences that he/she has experienced earlier.
Causes of Dissociative Identity Disorder
The cause of DID is still unclear but the psychological theory explains that this disease stems from severe traumatic experiences in childhood. Children who have been physically or sexually abused are more likely to develop dissociative identity disorder in adulthood. Additionally, people who have post-traumatic stress disorder and borderline personality disorder have a risk of developing dissociative identity disorder. It is a complex and chronic post-traumatic psychopathology closely related to severe, particularly early, child abuse.
Clinical Features
The main symptom of dissociative identity disorder (DID) is a person’s identity being involuntarily split between at least two distinct identities. The signs and symptoms include amnesia, two different personalities, blackouts, sleepwalking, automatic writing, social withdrawal, auditory hallucinations, inappropriate sexual behaviour, hostility, difficulty trusting others, referring to oneself as “we”. DID is characterized by the existence of two or more distinct personalities. One is the person’s usual (core) personality and others are known as alternate personalities or alters. The person may experience amnesia when an alter takes control over the person’s core personality. Other symptoms might include:
i. Dissociative Amnesia- This is a type of memory loss that involves disruption of memory, consciousness, identity and perception.
ii. Dissociative Fugue- It is reversible amnesia where a person loses awareness of his/her identity.
iii. Blurred Identity- This is a terrible situation for a person as it makes him/her helpless. The individual starts feeling like two or more people are talking in his head.
Treatment of Dissociative Identity Disorder
There are no specific drugs to cure this disorder, but treatment aims to integrate the disparate personalities back into a single personality. For this, the dominant personality must be made conscious of the existence of the other personalities.
i. Psychotherapy is the mainstay of the treatment of DID. The symptoms of DID must be closely observed and if a person frequently suffers from dissociative episodes, flashbacks, and self-destructive and suicidal impulses, the individual must be removed from all toxic environments that could trigger these dissociative behaviours. Individuals must learn to deal with dissociation and intense affects such as rage, terror, and despair through means of psychotherapy.
ii. Hypnosis is another mode of treatment that sometimes helps increase the information about the person who is suffering from DID, thereby increasing the control they have over those states when they change from one personality state to another.
iii. As DID is often associated with severe depression, electroconvulsive therapy (ECT) can be a viable treatment when the combination of psychotherapy and medication fails to relieve symptoms.
As the origin of dissociative identity disorder in most individuals remains related to exposure to traumatic events, prevention for this disorder involves minimizing the exposure to traumatic events and helping survivors come out of it in a healthy way.
The lack of specific drug treatment and the rewarding outcome of psychotherapy in dissociative disorders make these clinical phenomena an avenue for innovation in psychiatry. Nevertheless, this avenue is promising for further illumination of the operations of the human mind when unexpected deviations of external reality challenge its capacity for adaptation and survival.