Obesity is associated with metabolic disturbances that usually is the reason for tissue stress and dysfunction. The recent findings have highlighted the substantial impact that obesity and MetS parameters have on immunity and pathogen defense, involving the disruption of lymphoid tissue integrity, alterations in leukocyte development, phenotypes, and activity, and the coordination of innate and adaptive immune responses. Obese individuals are always at a greater risk for chronic disease and often present with clinical parameters of metabolic syndrome (MetS), insulin resistance, and systemic markers of chronic low-grade inflammation. It is known that cells of the immune system play an essential role in the pathogenesis of obesity and MetS-related chronic diseases, which is evidenced by leukocyte activation and dysfunction of metabolic tissues (adipose tissue, liver, pancreas, and the vasculature). Obesity shares with most chronic diseases, the presence of an inflammatory component, which accounts for the development of metabolic disease and other associated health alterations.
How Lipid Molecules Affect Immune Cells
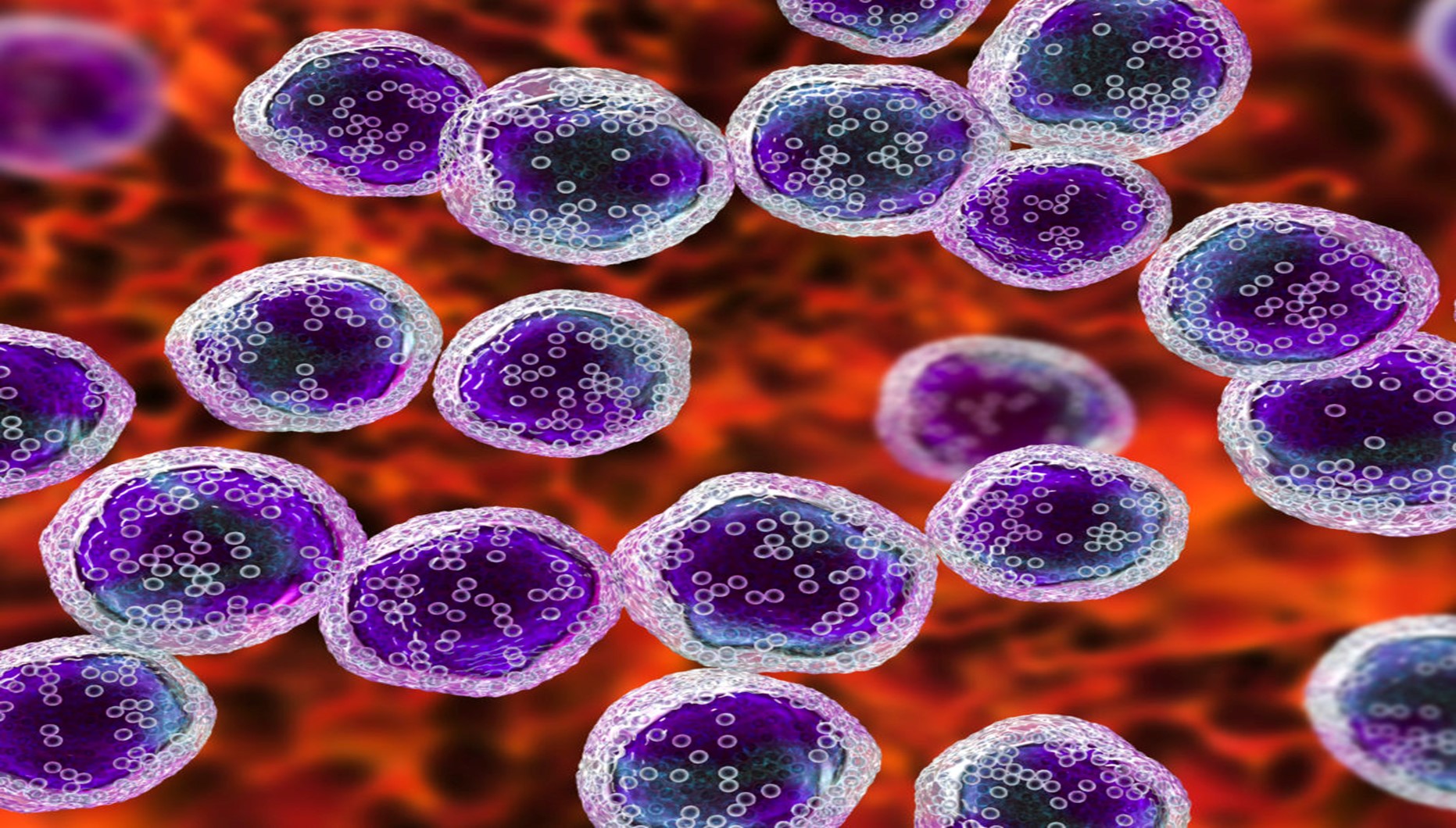
In certain metabolic disorders like obesity, immune cells interact with various classes of lipid molecules that are capable of controlling the plasticity of macrophages and the T lymphocytes. In addition to the adipocyte, the microenvironment of adipose cells consists of several other cells central to the health of the tissue, that are involved in the pathogenesis of obesity. These cell types include pre-adipocytes, endothelial cells, fibroblasts, and immune cells; it does not preclude the importance of other stromal constituents. As an individual gradually becomes obese, there is a dramatic increase in M1 macrophages into adipose tissue. As the accumulation of lipid molecules continues within the adipose tissue both in adipocytes and macrophages, there is a shift in macrophage subtype to a pro-inflammatory, M1 polarization.
The inflammatory state in obesity is reflected in increased circulating levels of pro-inflammatory proteins; it also occurs in adolescents and children, along with the occurrence in adults. However, it is known that obesity itself (diet or genetic induced) decreases immunity leading to increased risk of bacterial and viral infection as well as decreased responsiveness to some vaccinations. There is always a metabolic tug-of-war between tumor cells and T cells that changes in humans with obesity. The research revealed that tumors grow rapidly in animals on high-fat diets compared to those on normal diets. Additionally a high-fat diet reduces the numbers and anti-tumor activity of CD8+ T cells (a type of immune cells inside tumors), which occurs because cancer cells reprogram their metabolism in response to increased fat availability to better gobble up energy-rich fat molecules, this depletes the tumor microenvironment of certain fatty acids, depriving T cells of fuel and accelerating tumor growth. Obesity enhances the cancer cells to outcompete tumor-killing immune cells in a battle for fuel. Several experiments revealed that diet-related differences in tumor growth were specifically dependent on the activity of CD8 + T cells, immune cells that can attack and destroy cancer cells.
This phenomenon is seen in cancer types that are immunogenic, that contain high number of immune cells which can be easily recognized by the immune system and are more likely to provoke an immune response. A better understanding and management of obesity is required among people. Finding suggests, that blocking the fat-related metabolic reprogramming significantly can reduce tumor volume in mice having high-fat diets. Since CD8+ T cells are considered the main weapon used by immunotherapies that can activate the immune system against cancer. Cancer cells do so by rewiring their metabolisms to increase fat consumption. Blocking this rewiring enhances anti-tumor immunity. New strategies suggest targeting cancer metabolism and improve immunotherapies. This finding follows that a therapy that would potentially work in one setting might not be as effective in another.