Received: Wed 14, Sep 2022
Accepted: Sat 24, Sep 2022
Abstract
Middle-aged male known case of hypothyroidism presented with shortness of breath and hypoxia. Echo showed large RA myxoma with ASD causing right to left shunt.
Keywords
atrial myxoma; right to left shunt; transesophageal echo; atrial septal defect
1. Introduction
Myxomas are the most common primary cardiac neoplasm in adults; they may occur in any chamber. Left atrium is the most common site (75%), and the right atrium (10-20%) being second in number [1]. The association of myxoma with congenital cardiac disease is rare [2]. The presentation of right atrial myxoma include ascites, hepatomegaly, peripheral edema due to right heart failure. Sometime patients present with pulmonary embolism. Vague symptoms of malaise, weight loss and fever may also be present. We report a case of young male who presented with dyspnea and hypoxia. The 2D and transesophageal echo showed large RA myxoma with right to left shunting across inter atrial septum.
2. Case Report
37-year male known case of hypothyroidism and family history positive for premature CAD presented with shortness of breath on mild exertion (NYHA III) for last 1 year with worsening of symptoms for last 6 months (NYHA III-IV). No history of chest pain, presyncope or syncope. On examination his BP was 105/67mmhg and heart rate was 88 beats/minute, RR was 18 breath/minute, So2 80% at room air, he was Afebrile, JVP was elevated, and clubbing was +ve (Figure 1). Cardiac auscultation was unremarkable.
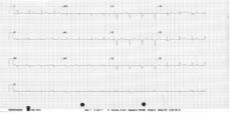
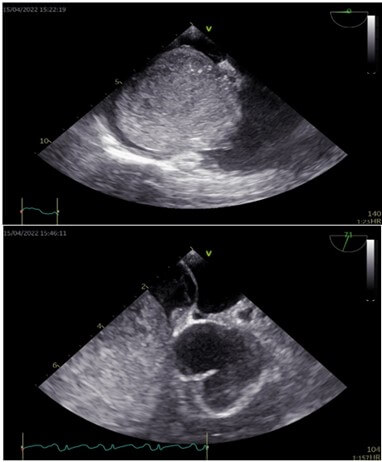
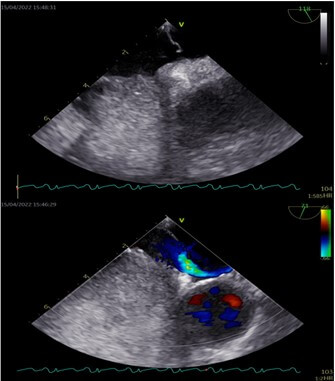
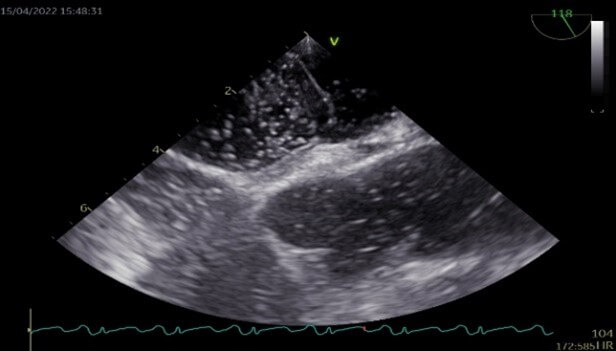
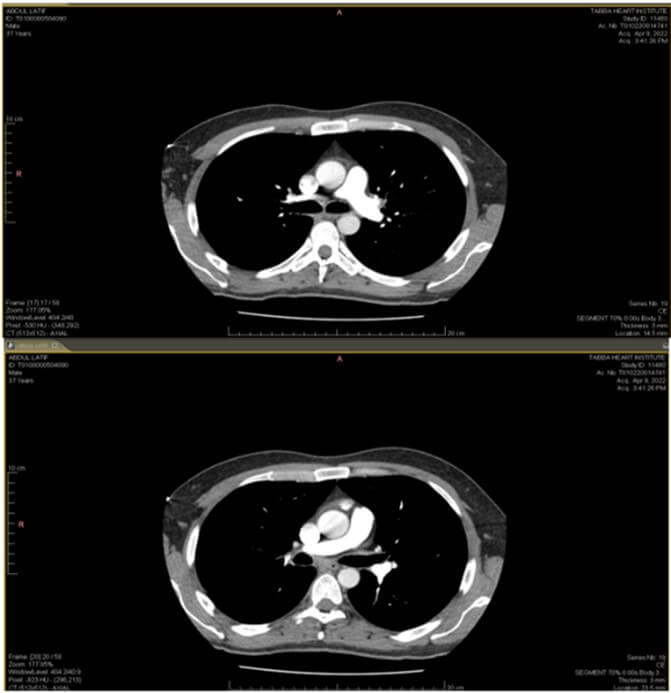
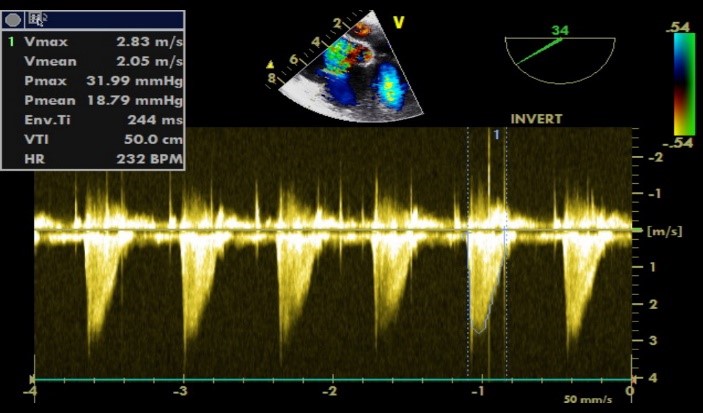
ECG showed sinus rhythm with normal intervals (Figure 2). Transthoracic echocardiography done showed normal LV function, severe dilated RA, large RA myxoma 40 × 50 mm almost filling whole RA and obstructing tricuspid valve. Normal size RV with mild right ventricular (RV) dysfunction –TAPSE 15mm. In view of low So2 CTPA done to rule out pulmonary embolism. PE was ruled out by CTPA (Figure 6). Transesophageal echocardiography done showed severely dilated right atrium, large echogenic well circumscribed mass measures 62 × 62 mm in diameter filling most of right atrium suggestive of Myxoma with small 6mm ASD causing right to left shunting confirmed on bubble contrast study (Figures 3-5). Patient admitted for RA myxoma resection. His baseline workup showed haemoglobin of 19.9g/dl with hematocrit of 64%. Arterial blood gases showed pH: 7.46, pO2: 44mmhg, pCO2: 23mmhg, HCO3: 16, saturation of 78%. Patient was on 5lit O2. Chest x-ray was normal.
Hematology consult was taken for polycythemia, advised therapeutic phlebotomy. Two 400ml therapeutic phlebotomy was done for target hematocrit of 55%. Patient sent for surgery, RA myxoma resected (Figures 9 & 10) with ASD patch closure. Intra OP TEE done post myxoma resection and ASD patch closure showed well resected RA myxoma with no residual shunt across interatrial septum, severe non-coapting tricuspid regurgitation (Figures 7 & 8) secondary to dilated annulus noted with no gradient across the valve, tricuspid valve annuloplasty done.

Postoperatively in ICU patient became hypotensive despite of escalated inotropic and vasopressor support. Transthoracic echocardiography done showed severe right ventricular dysfunction. In view of persistent hypotension heart team was called and decided to proceed with Cavo - pulmonary shunt (Glenn) to rest and recover right ventricle. Patient recovered well post Glenn shunt, RV function improved significantly. After 14 days of hospital stay patient discharged home in stable condition.

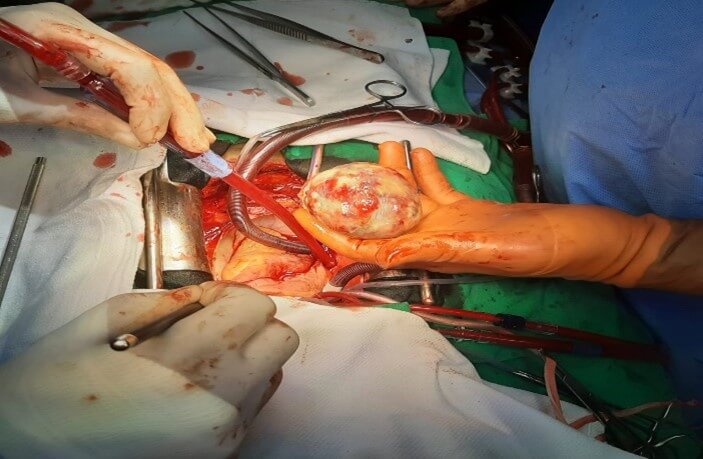
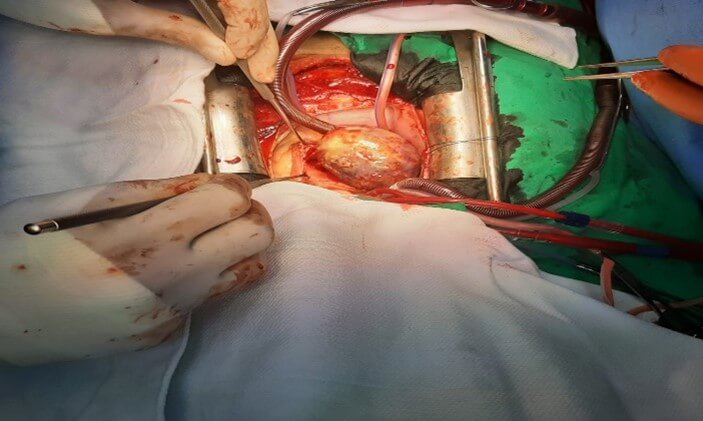
Specimen - Gross specimen consists of a single, irregular, grey-white to light brown, nodular tissue piece measuring 6 × 5 × 4 cm (Figure 11). Histopathology examination revealed a neoplastic lesion composed of spindle to stellate shaped cells arranged singly and in clusters embedded in abundant myxoid stroma.

3. Discussion
Right atrial myxoma with right to left shunt is very rare. Till now only few cases of right atrial myxoma associated with atrial septal defect and polycythemia have been reported [2]. Patients usually present with signs and symptoms of right heart failure and pulmonary embolism. Our patient had raised JVP but no peripheral edema, ascites or hepatomegaly. Pulmonary embolism was ruled out with CTPA. He had NYHA III symptoms for 18 months and was hypoxic on presentation. Echo showed large RA myxoma. The hypoxia was thought to be from the partial obstruction of the tricuspid valve due to the massive RA myxoma and subsequent elevation of the right atrial pressure leading to right-to-left shunt through the ASD.
Echocardiographically there are two distinct types of myxomas: i) spherical type characterized by a solid, round shape with non-mobile surface (52%) and ii) polypoid type characterized by soft and irregular shape with mobile surface (48%) [3]. Right atrial myxomas tend to have a broad-based attachment to the atrial wall or septum [4]. In our patient it was solid, round shape with non-mobile surface.
Surgical resection is the definitive treatment. In our case we also performed ASD patch closure and TV repair due to severe non-coapting tricuspid regurgitation secondary to dilated annulus. Patient post op had severe right ventricular dysfunction, was on maximum inotropic support, which was difficult to taper off, probably because the right ventricle was not habitual of large volume of blood from right atrium as giant myxoma was obstructing tricuspid valve. Right Cavo-pulmonary shunt (Glenn) was done to allow right ventricle to rest and recover. Patient recovered well post Glenn shunt, inotropic support tapered off, RV function improved significantly. After 14 days of hospital stay patient discharged home in stable condition.
REFERENCES
[1] Sumit Mittle, Amgad
N Makaryus, Loukas Boutis et al. “Right-sided Myxomas”. J Am Soc
Echocardiogr, vol. 18, no. 6, pp. 695, 2005. View at: Publisher
Site | PubMed
[2] Murayama H, Tamaki S, Kato N et al. “Right
atrial myxoma associated with atrial septal defect: a case report and review of
the literature.” Ann Thorac Cardiovasc Surg, vol. 7, no. 3, pp. 166-169
2001. View at: Publisher
Site | PubMed
[3] Jong-Won Ha, Woong-Chul Kang, Namsik Chung et al. “Echocardiographic and morphologic characteristics of left atrial myxoma and their relation to systemic embolism.” Am J Cardiol vol. 83, no. 11, pp. 1579-1582, 1999. View at: Publisher Site | PubMed
[4] Kirklin JW, Barratt-Boyes BG “Cardiac Surgery”. New York: Churchill Livingstone, Cardiac tumor, pp. 1635-1653, 1993. View at: Publisher Site
