Received: Fri 18, Sep 2020
Accepted: Mon 26, Oct 2020
Abstract
Introduction: Cystic brain lesions represented a rare finding in cancer patients, even more uncommon in rare disease as neuroendocrine neoplasms.
Patient Presentation: We presented a case of a patient with neurologic symptoms as first and only presentation of a neuroendocrine tumor of the lung.
Management and Outcome: First of all, the patient underwent neuroradiologic assessment with the finding of cystic brain lesions. A chest and abdomen CT scan detected a pulmonary lesion; a biopsy of this mass revealed an atypical carcinoid of the lung. Considering the absence of other symptoms, in order to clarify the nature of the cystic brain lesions, a right frontal craniotomy was performed, and a cyst was completely excised. Pathology confirmed the metastatic nature of the brain lesions. Unfortunately, the conditions of the patient quickly worsened, and he passed away before the start of the treatment.
Conclusion: Due to the low awareness about neuroendocrine tumors and their clinical and radiological presentations, multidisciplinary approach can represent the cornerstone to provide an accurate and timely diagnosis.
1. Introduction
Lung carcinoids are a subcategory of neuroendocrine neoplasms (NENs) that represents 1-2% of all pulmonary malignancies and is divided into typical and atypical, the latter being the rarest(10%) [1]. Brain metastases are an uncommon event in advanced well-differentiated NENs (1.5-5%) but the risk rises to 10-35% in cases of lung carcinoids [2]. The radiologic evidence of multiple cystic lesions of the brain is an uncommon event that needs to be considered carefully to avoid a misdiagnosis between metastases and parasitic infections. Moreover, neoplasms and antitumoral treatments are known to increase the risk of infections. Here we reported the case of a patient that first presented neurological symptoms due to cystic brain lesions from a lung atypical carcinoid (AC), aiming to highlight the multidisciplinary key role in differential diagnosis. To the best of our knowledge, the cases of brain metastases from lung carcinoids that first presented with neurologic symptoms are six [3-8], and only one of them with a completely cystic aspect.
2. Patient Presentation
In March 2019, a 57-year old man developed mood swings and outbursts, but this behaviour was considered related to his work problems and temper. No fever, cough or other symptoms were reported. He was a smoker since a young age (35 pack years) and suffered from hypertension. No work-related factors of infections risk or travel to tropical countries were reported. His wife recalled the assumption of raw meat in March 2019. In December 2019, due to worsening of his clinical profile, a brain magnetic resonance imaging (MRI) was performed (Figure 1).
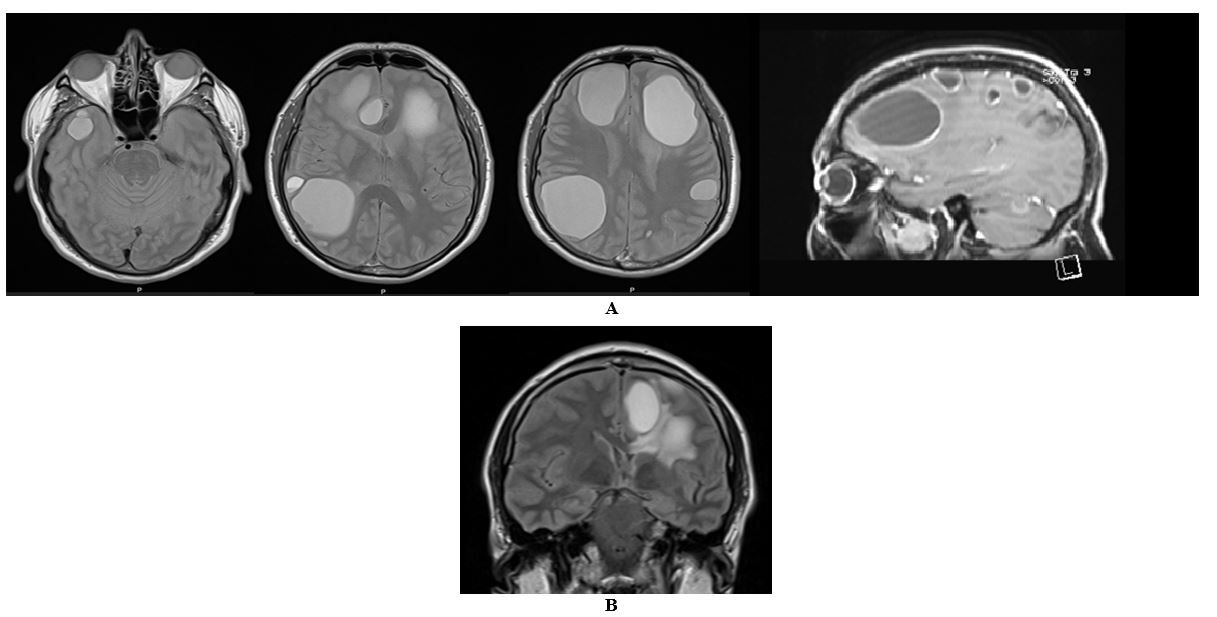

Multiple supratentorial and infratentorial lesions were identified with compression on the surrounding brain structures. Few oedema between frontal lesions was reported (Figure 1B). A chest and abdomen computer tomography (CT) scan was performed, revealing a right lung lesions(3x3cm) with a large mediastinal lesion which involved the main bronchi and the pulmonary vessels (8x9 cm) (Figure 2). A transbronchial ultrasound-guided needle aspiration led to the diagnosis of a lung NEN with proliferation index <2%. Platinum-based chemotherapy was proposed. The patient came to our Institute (European Neuroendocrine Tumor Society (ENETS) centre of excellence) for a second opinion. The revision by an expert pathologist in NENs confirmed the diagnosis of lung carcinoid, without mitoses or necrosis and with a Ki-67 of 2%.
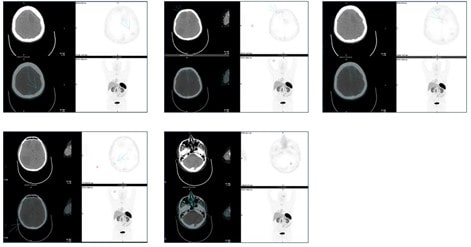
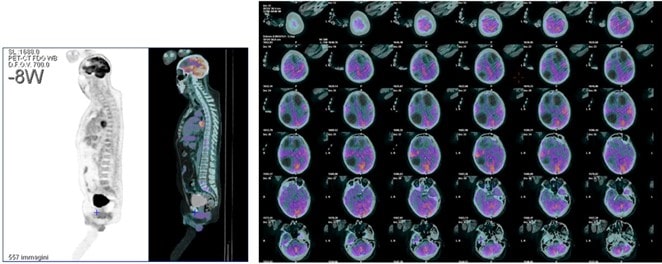
Clinical examination revealed a Karnofsky Performance Status Scale of 60%, bilateral oedema of lower limbs but no neurological signs. Infectious disease specialists and the neurosurgeons were involved in our multidisciplinary NET tumor board. The suggested tests (blood and cerebrospinal fluid (CSF) for bacteria and parasites) resulted negative and further radiological assessment were performed to complete the staging the diseases and to explore the brain lesions nature. A brain CT scan confirmed the presence of multiple supratentorial and infratentorial cystic lesions (up to 55 mm) with a rim enhancement, scarce perilesional oedema and a surrounding brain structures compression. A 68Gallium(Ga)-DOTATOC positron emission tomography (PET)/CT showed a low uptake of the radiotracer among brain lesions (Figure 3).
Blood test showed an ACTH-dependent hypercortisolism, suggesting a functioning NET, and metopirone therapy was started. Considering the pathologic features of the disease and the patient clinical pattern, the brain lesions were deemed the priority. Therefore, in order to define the brain lesions nature, a cyst was completely excised through a right frontal craniotomy: it appeared intact thick-walled and strictly adherent to the surrounding parenchyma. The pathological report indicated a likely diagnosis of lung AC metastases with a Mib-1 of 5-6/10hpf and without expression of ACTH.
3. Management and Outcome
Considering the predominance of neurological symptoms on the clinical pattern, brain pan-encephalic irradiation was proposed, delaying the start of a systemic treatment at a later time. In the main time, an integrated home care was activated but the clinical condition of the patient quickly deteriorated, and he died before starting the treatment.
4. Discussion
The purpose of this case report is to present an uncommon event in the setting of an already rare neoplastic disease and to underline the crucial role of the multidisciplinary involvement of all dedicated specialists in the diagnostic and therapeutic path. Indeed, in patients with an oncologic disease who develop brain lesions, the underestimation of the diagnostic process is one of the risks for the clinicians.
For this reason, we are used to discuss each NEN case in multidisciplinary team meetings in order to integrate the various expertise and experience, guidelines and evidence from the literature to offer each patient the best personalized treatment. Despite this, in the present case, the diagnostic definition of the brain cystic lesions was delayed due to the rarity of the event and the lack of knowledge about the primary disease. Indeed, the diagnosis was reached after almost one year from the development of neurologic symptoms. Furthermore, even when the diagnosis of the NENs is available, patients are often not addressed to a specialized centre, as happened in our case. Indeed, the patient came on his own initiative to our Institute as an ENETS centre of Excellence in NENs only after receiving the proposal of a first line treatment from another hospital.
Considering that, brain metastases can occur up to 35% of lung carcinoids [2] and the significant interval since the appearance of symptoms, the hypothesis of a metastatic nature of the cystic brain lesion could not be excluded. Several studies have reported cases of cystic brain metastases in non-neuroendocrine cancers, mainly non-small cell lung carcinomas (NSCLCs) with specific gene rearrangements [9, 10]. To the best of our knowledge, the cases of brain metastases from lung carcinoids that first presented with neurologic symptoms are six [3-8], and only one of them with a completely cystic aspect.
In our case, the assumption, without the certainty, of the metastatic nature of the brain lesions could have exposed the patient to the risk of a rapid worsening of his clinical conditions. Indeed, in accordance with the ENETS guidelines, a combination of radiotherapy and a systemic treatment with temozolomide could be considered for lung AC with brain metastases [11, 12]. Therefore, the collaboration with the infectious medicine specialist and neurosurgeons was key in excluding a possible infective cause. One of the most common causes of cystic lesions is zoonosis due to Echinococcus multilocularis which is found in the brain in 30% of cases [13]. Due to a slow growth of the hydatid cysts, the symptoms appear when they reach remarkable dimensions. As in our case, their radiologic features consist of a well-defined spherical shape, with a homogeneous fluid density at MRI and without peripheral oedema. Considering that only in 4% of cases of a primary brain echinococcosis IgG and IgE can be detected, the negative blood and CSF tests did not exclude this diagnosis. Neurocysticercosis was hypothesized. Indeed, the infection, due to Taenia Solium, could develop after eating raw meat (noted in medical history of our patient) and be associated to cystic brain lesions. The absence of the two pathognomonic radiologic features (the presence of the scolex and concurrent different evolution stages of the lesions [14]) and the negativity of the CSF test excluded this diagnosis. Furthermore, due the infective risk due to the ACTH-dependent hypercortisolism, the possibility of an advanced AC with a concurrent opportunistic infection was always open.
Barbone et al. recently described a case of lung cancer with brain metastases simulating neurocysticercosis. In this report, despite all serologic analyses, the diagnosis was finally reached with the pathologic analysis [15]. Similarly, only the biopsy clarified the metastatic nature of the brain lesions of our patient. Our case highlights the importance of an integrated collaboration between different experts especially in case of rare tumors and unusual images.
The multidisciplinary approach to rare neoplasms, which could mimic other pathologic conditions, represents the cornerstone to provide an accurate and timely diagnosis, ensure the implementation of appropriate treatment and to have a substantial impact on prognosis.
Acknowledgment
The authors thank Linda Ann Cairns for language revision.
Competing Interests
None.
Author Contributions
All authors contributed to the study conception and design. The first draft of the manuscript was written by Alice Laffi and revised by Francesca Spada. All the other authors commented on previous version of the manuscript. All authors read and approved the final manuscript.
Funding
None.
Data Availability Statement
Data sharing is not applicable to this article, as no new data were created or analysed in this study.
Disclaimer
The views expressed in the submitted article are authors’ own.
Ethical Approval
Not applicable.
Conflicts of Interest
None.
Code Availability
Not applicable.
REFERENCES
- Steuer CE, Behera M, Kim S, et al. “Atypical carcinoid tumor of the lung: a surveillance, epidemiology, and end results database analysis.” J Thorac Oncol, vol. 10, no. 3, pp. 479-485, 2015. View at: Publisher Site | PubMed
- Krug S, Teupe F, Michl P, et al. “Brain metastases in patients with neuroendocrine neoplasms: risk factors and outcome.” BMC Cancer, vol. 19, no. 1, pp. 362, 2019. View at: Publisher Site | PubMed
- Maiuri F, Cappabianca P, Del Basso De Caro M, et al. “Single brain metastases of carcinoid tumors.” J Neurooncol, vol. 66, no. 3, pp. 327-332, 2004. View at: Publisher Site | PubMed
- Hussein AM, Feun LG, Savaraj N, et al. “Carcinoid tumor presenting as central nervous system symptoms. Case report and review of the literature.” Am J Clin Oncol, vol. 13, no. 3, pp. 251-255, 1990. View at: Publisher Site | PubMed
- Greene KA, Anson JA, Martinez JA, et al. “Multicystic metastatic carcinoid to brain: case report.” J Neurooncol, vol. 17, no. 1, pp. 15-20, 1993. View at: Publisher Site | PubMed
- Porter DG, Chakrabarty A, McEvoy A, et al. “Intracranial carcinoid without evidence of extracranial disease.” Neuropathol Appl Neurobiol, vol. 26, no. 3, pp. 298-300, 2000. View at: Publisher Site | PubMed
- Nakamura Y, Shimokawa S, Ishibe R, et al. “Pulmonary carcinoid found in a patient who presented with initial symptoms of brain metastasis: report of a case.” Surg Today, vol. 31, no. 6, pp. 510-512, 2001. View at: Publisher Site | PubMed
- Sundar IV, Jain SK, Kurmi D, et al. “Malignant metastatic carcinoid presenting as brain tumor.” Asian J Neurosurg, vol. 11, no. 3, pp. 314, 2016. View at: Publisher Site | PubMed
- Grubb WR, Machtay M, Dowlati A, et al. “Diffuse Atypical Cystic Brain Metastases in ALK+ NSCLC Treated With Whole Brain Radiation and Second-Generation ALK-Targeted Therapy.” Pract Radiat Oncol, vol. 9, no. 2, pp. e129-e133, 2019. View at: Publisher Site | PubMed
- Marta GN, da Cunha Colombo Bonadio RR, Martins RE, et al. “Cystic brain metastases in ALK-rearranged non-small cell lung cancer.” Ecancermedicalscience, vol. 12, pp. 818, 2018. View at: Publisher Site | PubMed
- Caplin ME, Baudin E, Ferolla P, et al. “Pulmonary neuroendocrine (carcinoid) tumors: European Neuroendocrine Tumor Society expert consensus and recommendations for best practice for typical and atypical pulmonary carcinoids.” Ann Oncol, vol. 26, no. 8, pp. 1604-1620, 2015. View at: Publisher Site | PubMed
- Pavel M, Grossman A, Arnold R, et al. “ENETS consensus guidelines for the management of brain, cardiac and ovarian metastases from neuroendocrine tumors.” Neuroendocrinology, vol. 91, no. 4, pp. 326-332, 2010. View at: Publisher Site | PubMed
- Hilmani S “Brain hydatid cyst.”
- Del Brutto OH, Rajshekhar V, White AC Jr, et al. “Proposed diagnostic criteria for neurocysticercosis.” Neurology, vol. 57, no. 2, pp. 177-183, 2001. View at: Publisher Site | PubMed
- Barbone F, Peri M, Vitale M, et al. “Atypical radiological presentation of multiple cystic brain metastases from lung cancer simulating neurocysticercosis.” BMJ Case Rep, vol. 12, no. 10, pp. e231678, 2019. View at: Publisher Site | PubMed
