Received: Sat 05, Sep 2020
Accepted: Mon 12, Oct 2020
Abstract
Introduction: Low back pain is rarely the first manifestation of malignancy. The symptoms may be exacerbated by coexisting inflammation and subside after antibiotic therapy. Such a clinical course may lead to a delay in the diagnosis of cancer.
Case Description: 65-year-old smoking man was admitted to the Neurology Department with severe low back pain and increased serum levels of inflammatory markers. The chest X-ray was normal. Due to repeated complaints, a wide range of diagnostics of the lesion was performed. An isolated irregular infiltration penetrating the intervertebral foramina and involving the L5 spinous process and the right dorsal extensor muscle along the vertebral arch, in a total size up to 3.5 cm, in addition to the degenerative disc changes, was visualized in magnetic resonance imaging (MRI). Prolonged antibiotic therapy resulted in a significant decrease in CRP and clinical improvement. During the second exacerbation of the refractory back pain in the L-S and Th regions after 15 months, the pathological structures initially diagnosed as inflammatory infiltrations were finally recognized as a metastatic infiltration of squamous cell carcinoma (SCC) of the lung. The CT examination to the chest demonstrated a large irregular tumor in the right lung.
Conclusion: The reported rare case of SCC non-small cell lung cancer metastasis to the lumbar and presacral spinal region shows limited usefulness of MRI to give a specific diagnosis of such infiltration. Despite the rarity of tumors at this site, an invasive diagnostic method should be considered first with any unclear changes.
1. Introduction
Low back pain (lumbar back pain) is defined as pain in the back from the level of the lowest rib down to the gluteal fold, with or without radiation into the legs [1]. An episode of low back pain is called acute if it has arisen for the first time in a patient’s life, or after a pain-free interval of at least six months and lasts no longer than six weeks [2]. The majority of patients have a patho-anatomical relationship between low back pain and one or more pathological processes, including compression of neural structures, joint inflammation, and/or instability of one or more spinal motion segments [3]. Clinically relevant causes include disk herniation (4%), spinal stenosis (3%), spondylolisthesis (2%), vertebral body fracture (1-4%), ankylosing spondylitis (0.2%), spondylodiscitis (0.01%). In addition, in 0.7% of patients, low back pain is caused by malignancies (primary or metastatic) [4]. As much as 80-90% of cases have no clear findings in imaging [5].
We present a case of metastatic squamous cell carcinoma of the lung, causing infiltration of the lumbar and sacral spine regions with the initial clinical presentation of low back pain with infiltration in presacral region and sepsis.
2. Case Presentation
A 65-year-old smoking (10 cigarettes per day for the last 40 years) male was admitted to the Neurological Ward (25th July 2017) with severe low back pain without body mass decline during the previous 6 months (BMI = 31.0). Neurological examination revealed sciatica symptoms on the left side and tenderness during palpation of the aforementioned region. Paresis and asymmetry of the lower limb reflexes were noted. Laboratory tests showed increased serum concentration of C-reactive protein (CRP) - 43.9 mg/dL (normal range < 5 mg/dL), without neutrophilia. Initial blood and urine cultures were negative. The chest X-ray was normal. Antibiotic therapy (Cefuroxime) was started, with no clinical improvement and a further increase in CRP up to 268.2 mg/dl on the 7th day of hospitalization.
The repeated blood culture on the 9th day was positive with grow of Acinetobacter lwoffii. Further blood tests (total blood count, biochemical and neoplastic markers: prostate-specific antigen, carcinoembryonic antigen and carbohydrate antigen 19-9 tests) were normal. Computed tomography (CT) of the thoracic, lumbar and sacral spine regions (Th-L-S) revealed no significant pathology. Ultrasound showed an enlarged liver (17 cm) and splenomegaly (17 cm in length) with a normal sonography structure. Magnetic resonance imaging (MRI) performed on 3rd August, visualized irregular infiltration penetrating the intervertebral foramina and involving the L5 spinous process and the right dorsal extensor muscle along the vertebral arch, in a total size up to 3.5 cm, in addition to the degenerative disc changes (Figures 1A & 1B).

Consulting neurosurgeon considered these changes as inflammatory and suggested antibiotic therapy. Despite the intravenous administration of high doses of meropenem and amikacin, the patient’s general conditions deteriorated with the development of acute respiratory failure requiring mechanical ventilation in the Intensive Care Unit. The MRI of the brain was unremarkable. The antibiotic therapy was continued for 7 days, followed by clinical improvement with a significant decline in CRP (15.8 mg/dL). The repeated MRI of the L-S spine, after 14 days, showed a slight regression of the previously visualized lesions but revealed a new infiltration in the presacral region (length 11 cm and thickness 2.1 cm). Continued antibiotic therapy (Meropenem) resulted in a significant decrease in CRP and clinical improvement.
The patient was discharged home after 44 days (7th September) with a recommendation for rehabilitation and regular neurological checkups. After 15 months (December 2018), the patient was referred by his family doctor to the neurological ward due to severe exacerbation of the back pain in the L-S and Th regions nonresponding to nonsteroidal anti-inflammatory drugs and tramadol. There was a 20 kg body mass wasting (22% of the initial body mass for 15 months) due to the loss of appetite. Blood tests revealed leukocytosis (17.0 K/µL (normal range 4.3-10.2) with moderate increase in CRP (19.4 mg/dL) but normal procalcitonin level (0.06 mg/dL). In the following days, a rise in serum CRP levels was observed.
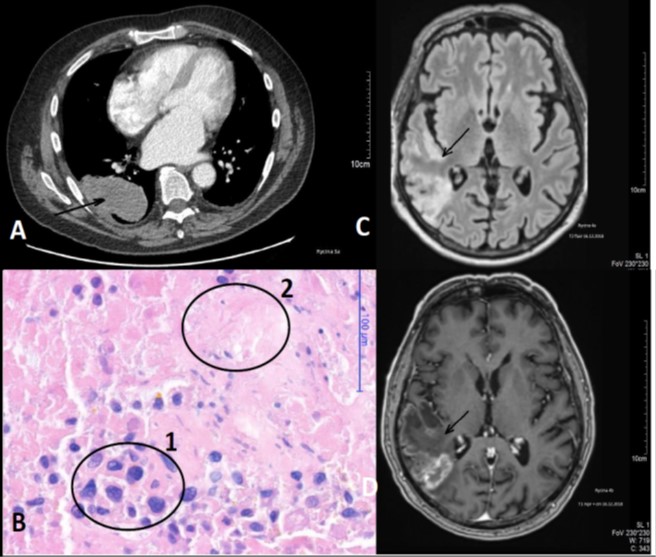
Empiric antibiotic therapy (Meropenem, Ceftriaxone, Vancomycin) was started. Due to behavioural changes such as increased suspicion and episodes of aggression, a head MRI scan was performed, visualizing ischaemic changes in the posterior part of the right parietal and temporal lobes (Figures 2C & 2D). The CT examination was extended to the chest, abdomen and pelvis, which demonstrated a large irregular structure (8.5 x 5.5 x 7.5 cm) in the 9 and 10 segments of the right lung and infiltrative lesions of the thoracic spine (Figure 2A). The MRI (6th December) confirmed the infiltration of peri-vertebral soft tissues, spanning from Th 9 to Th 11 vertebrae and penetrating into the spinal canal (Figures 1C & 1D). Pathological examination of surgically obtained tissue showed infiltration of the squamous cell carcinoma (SCC) (Figure 2B). Best supportive care of non-small cell lung cancer (NSCLC) was the only treatment due to poor clinical status. The patient died two months later.
3. Discussion
The mechanism of pain in degenerative disease is often of unknown origin [5, 6]. Differential diagnoses of back pain, leg pain, or hip pain include lumbar disk herniation, lumbar spinal canal stenosis or hip osteoarthritis. However, in daily clinical practice, the prevalence of these clinical conditions is relatively low [7-9], and sometimes the source of the pain cannot be readily identified. Other causes of lumbago, such as degenerative disk disease and degenerative facet syndrome, are difficult to identify as the sources of pain because the diagnosis is usually resource-intensive, with the high cost and the risk of proper diagnosis and management. As a result of these factors, undiagnosed back or leg pain is widespread in daily clinical practice; consequently, it remains a great need for improvement in pain management systems. Lumbar and presacral tumors are uncommon, which occurs estimated at 1 for 40,000-63,000 patients, and 60% of presacral tumors are congenital [10].
The spine accounts for 80% of metastatic bone lesions and is one of the most common sites for the early presentation of metastases [11, 12]. Cancer of the breast, lung, and prostate are the most common causes of bony metastases, and up to 50% of patients with these types of cancers develop bone metastases [11, 13]. However, the majority of skeletal metastases are asymptomatic; cervical and lumbar metastases are more symptomatic than those in the thoracic spine [13, 14].
Usually, the metastatic disease is widespread by the time of patients’ referral to the hospital [15]. Our patient did not complain of typical clinical signs of NSCLC (dyspnoea, change in the nature of the cough or hemoptysis, weight loss, fever) as well as from the other organs, although he smoked 10 cigarettes per day for the last 40 years (20 pack-years). The chest X-ray was normal at the time of the initial presentation. After 17 months, CT scan of the chest revealed a large irregular mass of the right lung, the primary tumor, corresponding to the SCC with the infiltration in the peri-vertebral soft tissues, spanning from Th 9 to Th 11.
An initial inflammatory mask of the neoplastic process, clinical improvement after antibiotic therapy caused the delay in the proper diagnosis. So, we think it was one of the rarer cases of metastatic SCC to the lumbar and presacral spinal region. Due to poor clinical condition, it was too late for oncological therapy.
4. Conclusion
The reported rare case of SCC metastasis to the lumbar and presacral spinal region shows limited usefulness of MRI to give a specific diagnosis of such infiltration. In addition, the coexisting inflammatory process and the improvement of symptoms after antibiotic therapy weakened oncological alertness and caused the delay in the diagnosis. Despite the rarity of tumors at this site, an invasive diagnostic method should be considered first with any unclear changes.
Funding
None.
Ethical Approval
As a case report without Protected Health Information, no ethics approval was required for this project.
Consent
Written informed consent was not obtained from the patient for publication of this case report and accompanying images. We have a copy of the written consent of the patient's wife. The written consent is available for review by the Editor-in-Chief of this journal.
Competing Interests
None.
Author Contributions
DB, TT, ASW, and DL had a clinical management of this patient. DB drafted the manuscript, did first selection of articles, and assessed the quality of the papers. JC revised the manuscript critically. All authors read and approved the final manuscript.
REFERENCES
- Deutsche Gesellschaft für Allgemeinmedizin, Familienmedizin (DEGAM) Kreuzschmerzen “Düsseldorf: DEGAM. (DEGAM-Leitlinie:3). www.degam.de/files/Inhalte/Leitlinien-Inhalte/Dokumente/DEGAM-S3-Leitlinien/LL-03_Kreuz_mod-007.pdf.” 2003.
- Nationale Versorgungs. Leitlinie Kreuzschmerz http://www.leitlinien.de/mdb/downloads/nvl/kreuzschmerz/kreuzschmerz-1aufl-vers5-lang.pdf
- Casser HR, Seddigh S, Rauschmann M “Acute Lumbar Back Pain.” Dtsch Arztebl Int, vol. 113, no. 13, pp. 223-234, 2016. View at: Publisher Site | PubMed
- Deyo RA, Weinstein JN “Low back pain.” N Engl J Med, vol. 344, no. 5, pp. 363-370, 2001. View at: Publisher Site | PubMed
- Koes BW, van Tulder MW, Thomas S “Diagnosis and treatment of low back pain.” BMJ, vol. 332, no. 7555, pp. 1430-1434, 2006. View at: Publisher Site | PubMed
- Litwic A, Edwards MH, Dennison EM, et al. “Epidemiology and burden of osteoarthritis.” Br Med Bull, vol. 105, pp. 185-199, 2013. View at: Publisher Site | PubMed
- Suzuki H, Kanchiku T, Imajo Y, et al. “Diagnosis and Characters of Non-Specific Low Back Pain in Japan: The Yamaguchi Low Back Pain Study.” PLoS One, vol. 11, no. 8, pp. e0160454, 2016. View at: Publisher Site | PubMed
- Ishimoto Y, Yoshimura N, Muraki S, et al. “Prevalence of symptomatic lumbar spinal stenosis and its association with physical performance in a population-based cohort in Japan: the Wakayama Spine Study.” Osteoarthritis Cartilage, vol. 20, no. 10, pp. 1103-1108, 2012. View at: Publisher Site | PubMed
- Goldie I “Att förebygga sjukdomar i rörelseorganen.” Socialstyrelsen, 14: 129–39, 1987.
- Jao SW, Beart RW Jr, Spencer RJ, et al. “Retrorectal tumors. Mayo Clinic experience, 1960-1979.” Dis Colon Rectum, vol. 28, no. 9, pp. 644-652, 1985. View at: Publisher Site | PubMed
- Lote K, Walloe A, Bjersand A “Bone metastasis. Prognosis, diagnosis and treatment.” Acta Radiol Oncol, vol. 25, no. 4-6, pp. 227-232, 1986. View at: Publisher Site | PubMed
- Nielsen OS, Munro AJ, Tannock IF “Bone metastases: pathophysiology and management policy.” J Clin Oncol, vol. 9, no. 3, pp. 509-524, 1991. View at: Publisher Site | PubMed
- Schaberg J, Gainor BJ “A profile of metastatic carcinoma of the spine.” Spine (Phila Pa 1976), vol. 10, no. 1, pp. 19-20, 1985. View at: Publisher Site | PubMed
- Krishnamurthy GT, Tubis M, Hiss J, et al. “Distribution pattern of metastatic bone disease. A need for total body skeletal image.” JAMA, vol. 237, no. 23, pp. 2504-2506, 1977. View at: PubMed
- Stoll BA “Natural history, prognosis, and staging of bone metastases.” Bone metastases: monitoring and treatment New York, NY, USA: Raven, pp. 1-20, 1983.
