Received: Wed 12, Aug 2020
Accepted: Thu 27, Aug 2020
Abstract
Pott’s puffy tumor is a non-neoplastic, Otolaryngological emergency. It is regarded as a rare clinical condition in the post-antibiotic era and a high index of suspicion is required for its diagnosis. The aetiology is multifactorial and includes sinusitis, infections, trauma, surgery, malignancy, substance abuse as well as contiguous spread along neurovascular bundles. These result in osteomyelitis and subperiosteal abscess formation within the frontal bone. Intracranial involvement can also occur and lead to serious complications. This is the case report of a 12-year old female who developed intermittent forehead swelling, headaches and pyrexia over a 2-week period. Radiological imaging identified changes consistent with a Pott’s puffy tumor complicated by an intracranial abscess. A combined open and endoscopic endonasal approach was used to drain the purulent collections and the patient was placed on antibiotics for a total of six weeks. The management of Pott’s puffy tumor will then be discussed.
1. Introduction
Pott’s puffy tumor has been infrequently reported since the widespread use of antibiotics for head and neck infections [1, 2]. As a result, it is not a common differential diagnosis for frontal headaches and a high suspicion has to be maintained in order to diagnose and treat the condition. It is a complication of frontal sinus infection and can be associated with intracranial spread as well as mortality rates as high as 16% [3-5]. A combination of medical and surgical management is necessary in order to treat this uncommon condition.
2. Case Report
This is the report of a 12-year-old female, who presented to the Eric Williams Medical Sciences Complex (Trinidad, West Indies) complaining of a fluctuating forehead swelling, intermittent frontal headaches and a low-grade pyrexia of a two week duration. Her parents stated that the forehead swelling was initially significant but then decreased in size over the previous ten days. They further reported the occurrence of headaches four months previously. This was managed as an upper respiratory tract infection and had resolved following a week of broad-spectrum antibiotics (Co-amoxiclav). However, the headaches had returned intermittently a few weeks prior to presentation and this is what prompted them to seek medical attention. The headaches were described as mild and was not associated with nausea, vomiting or impaired consciousness. The patient had a past history of nasal congestion but no nasal discharge, epistaxis, anosmia, epiphora, post-nasal drip or allergic symptoms. There were no other significant otolaryngologic or neurological symptoms. There was no history of head trauma, insect bites or previous head surgery.
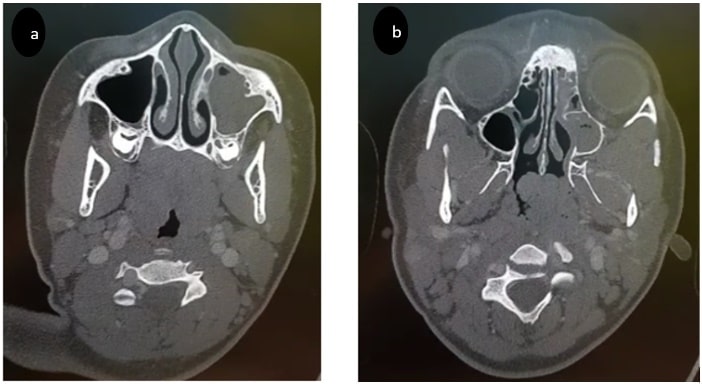
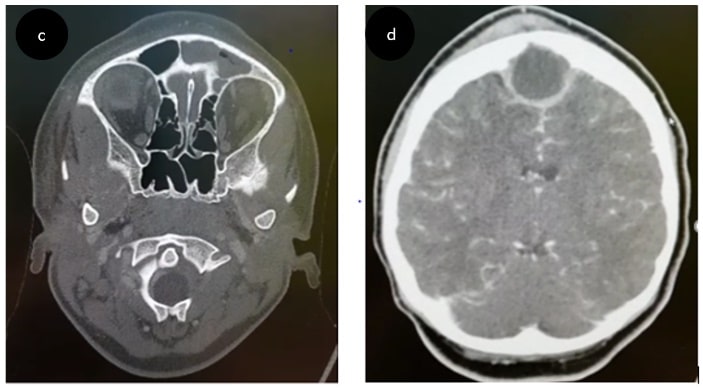
On general examination, the patient was well with minimal frontal swelling (Figures 1 & 2). The left frontal area was tender to palpation. The remainder of the ENT exam was normal. Endoscopic examination of the nose was not initially completed due to patient discomfort. Correspondingly, a working diagnosis of an inadequately treated frontal sinusitis was suspected. The patient was started on intravenous antibiotics (Co-amoxiclav and metronidazole) within the Emergency Department and a CT scan of the brain and paranasal sinuses was ordered due to the history of recurrent headaches, pyrexia and an elevated leucocyte count of 16 x 109 /L. This demonstrated opacification of the left frontal as well as the left ethmoid and left maxillary sinuses (Figures 3 & 4). There was oedema in the left frontal area. In addition, there was a large intracranial fluid collection consistent with a left frontal abscess (Figure 4). The walls of the involved sinuses appeared intact and there was no orbital involvement.


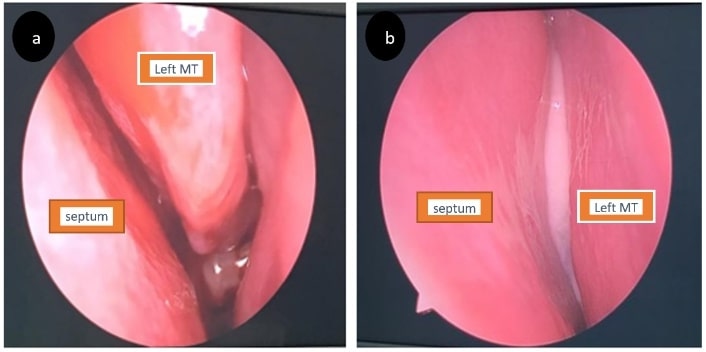
The patient was reviewed by both the Neurosurgery and Otolaryngology Departments and a diagnosis of Pott’s puffy tumor complicated by an intracranial abscess collection was made. Urgent surgical intervention was planned within 12 hours of admission. A combined open and endoscopic endonasal approach was utilized. An anterior craniotomy was initially performed via a burr hole and approximately 15 mL of purulent material was drained (Figure 5). Specimen was taken for microscopy, culture and sensitivity. The cavity was then irrigated. On endonasal endoscopic examination, the nasal mucosa appeared oedematous and pus was seen in the left middle and superior meati (Figure 6). Additionally, a left Draf 1 procedure, left uncinectomy and left middle meatal antrostomy was performed with sinus irrigation.

A CT scan carried out on the second postoperative day confirmed resolution of the intracranial collection. The wound swab had grown a combination of staphylococcus aureus and Klebsiella. The patient was kept hospitalized for a period of ten days, maintained on parenteral Co-amoxiclav and metronidazole which were in keeping with the microbiological sensitivities. An uneventful recovery with complete resolution of the headaches ensued and the patient was discharged from the ENT department after 6 weeks of oral antibiotics.
3. Discussion
Pott’s puffy tumor is a rare complication of sinusitis that is characterized by osteomyelitis of the frontal bone with corresponding sub-periosteal abscess formation that may be intra or extra cranial or indeed both. It is named after Sir Percival Pott who first described the condition in 1768 in relation to frontal head trauma [6]. Additional underlying causes have since been identified and include acute sinusitis, chronic sinusitis, periorbital infection, mastoid infection, insect bites, acupuncture, malignancy, head trauma, craniotomy, infected skull implants, intracranial infection and intranasal substance abuse [7-9].
Oedema from inflammation of the subgaleal tissues causes the ‘puffy’ forehead appearance. However, the swelling may extend anteriorly as far down as the eyebrow and can present as a periorbital swelling in approximately 30% of patients [10, 11]. In the case described, the swelling had started to resolve by the time the patient was brought to the hospital. The usual complaints are headache, photophobia, pyrexia, nasal congestion and nasal discharge [8, 12]. Tenderness on palpation over the affected frontal sinus (as elicited with our patient) may also be observed [8].
Extension through the posterior frontal sinus wall can also occur and cause intracranial complications as occurred in this patient. In 1995, Singh et al. reported on 219 patients that developed sinogenic intracranial complications [5]. These had included meningitis, subdural empyemas, epidural abscesses, intraparenchymal abscesses, dural sinus thrombosis and death. Symptoms suggestive of intracranial involvement include nausea, vomiting, lethargy, seizures and fluctuations in the level of consciousness [13]. Aside from headaches, the patient in this case report had no other symptoms suggesting intracranial spread.
The affected paranasal sinuses are the frontal sinuses. These attain their adult size around the time of adolescence [14, 15]. During puberty, extra sinus spread is more likely due to the rapid proliferation of the diploic vasculature without bony erosion. This can result in the spread of septic emboli from the mucosa of the obstructed frontal sinus through valve less veins to the marrow of the frontal bone or into the intracranial cavity [16, 17]. The patient in this report was adolescent and she had no obvious posterior frontal sinus wall erosion. Therefore, vascular spread may have been responsible for the intracranial abscess collection.
Polymicrobial growth is responsible for the sinus infection and includes microorganisms such as Streptococcus, Staphylococcus, Hemophilus influenzae and Klebsiella sp. [1, 7]. Intracranial infections additionally may contain anaerobic organisms [18]. Pathogens that have infrequently been cultured include Enterococcus, Pseudomonas, E. coli, P. multocida and S. constellatus [2, 11]. The culture in this case grew a combination of Staphylococcus aureus and Klebsiella sp. In addition to a high clinical suspicion - cross sectional imaging is necessary in order to assess the location, size and extent of disease as well as to detect the presence of intracranial involvement. CT or MRI scans can identify paranasal sinus opacification, frontal bone erosion, subcutaneous fat stranding, tissue oedema and the presence of a collection [19]. The use of contrast can further delineate the extent of intracranial involvement.
Both medical and surgical treatments are needed in order to successfully manage Pott’s puffy tumor. Urgent surgical drainage of the sinuses, abscess collections and removal of the infected bone is required. This can be accomplished via open (paranasal sinus trephination, external frontoethmoidectomy, craniotomy), endoscopic (Draf procedures, uncinectomy, middle meatal antrostomy) or combined approaches [8, 20]. In the case described, a combination approach was utilized because of the need to address intracranial involvement. Patients are also given broad spectrum antimicrobials over a 6-8 weeks period in order to address the frontal bone osteomyelitis and prevent a relapse [2, 9]. Once appropriately managed, full recovery can be expected.
4. Conclusion
Pott’s puffy tumor is an Otorhinolaryngological emergency. Though uncommon in the post-antibiotic era, a high degree of clinical suspicion is required if the diagnosis is not to be missed. Causative factors are multiple and can include: acute sinusitis, chronic sinusitis, periorbital infection, insect bites, acupuncture, malignancy, head trauma, craniotomy, infected skull implants, intracranial infection and intranasal substance abuse. Forehead swelling, headaches, photophobia, pyrexia, nasal congestion and nasal discharge are common presenting symptoms. Additional symptoms suggesting intracranial spread include nausea, vomiting, lethargy, seizures and fluctuations in the level of consciousness. The latter is associated with higher morbidity and mortality. A combination of medical and surgical management is necessary in order to treat this clinical rarity and preserve life.
Conflicts of Interest
None.
Financial Declaration
None.
REFERENCES
- V Raja, C Low, A Sastry, et al. “Pott's puffy tumor following an insect bite.” J Postgrad Med, vol. 53, no. 2, pp. 114-116, 2007. View at: Publisher Site | PubMed
- Hasan I, Smith SF, Hammond Kenny A “Potts puffy tumour: a rare but important diagnosis.” J Surg Case Rep, vol. 2019, no. 4, pp. rjz099, 2019. View at: Publisher Site
- Hitoshi Terui, Ikuko Numata, Yusuke Takata, et al. “Pott's Puffy Tumor Caused by Chronic Sinusitis Resulting in Sinocutaneous Fistula.” JAMA Dermatol, vol. 151, no. 11, pp. 1261-1263, 2015. View at: Publisher Site | PubMed
- Harpreet Singh Grewal, Neha Subhash Dangaych, Anthony Esposito “A tumor that is not a tumor but it sure can kill!” Am J Case Rep, vol. 13, pp. 133-136, 2012. View at: Publisher Site | PubMed
- B Singh, J Van Dellen, S Ramjettan, et al. “Sinogenic intracranial complications.” J Laryngol Otology, vol. 109, no. 10, pp. 945-950, 1995. View at: Publisher Site | PubMed
- “Observations on the Nature and Consequences of those Injuries to which the Head is liable from external Violence. Percival Pott (FRS).” Printed for L. Hawes, W. Clarke and R. Collins in Paternoster Row, London, MDCCLXXI.
- Chang Teng Wu, Jing Long Huang, Shao Hsuan Hsia, et al. “Pott's puffy tumor after acupuncture therapy.” Eur J Pediatr, vol. 168, no. 9, pp. 1147-1149, 2009. View at: Publisher Site | PubMed
- Pamela D Bannon, Robert F McCormack “Pott’s puffy tumor and epidural abscess arising from pansinusitis.” J Emerg Med, vol. 41, no. 6, pp. 616-622, 2011. View at: Publisher Site | PubMed
- Keehn B, Killeen Z, Jorgensen SA, et al. “Pott’s puffy tumor.” Appl Radiol, vol. 47, no. 3, pp. 30-31, 2018.
- A M S Morley “Pott's puffy tumour: a rare but sinister cause of periorbital oedema in a child.” Eye (Lond), vol. 23, no. 4, pp. 990-991, 2009. View at: Publisher Site | PubMed
- Bih Yu Tsai, Kuang Lin Lin, Tzou Yien Lin, et al. “Pott’s puffy tumor in children.” Childs Nerv Syst, vol. 26, no. 1, pp. 53-60, 2010. View at: Publisher Site | PubMed
- Figen Bakirtas Palabiyik, Zeynep Yazici, Benhur Cetin, et al. “Pott Puffy Tumor in Children: A Rare Emergency Clinical Entity.” J Craniofac Surg, vol. 27, no. 3, pp. 313-316, 2016. View at: Publisher Site | PubMed
- Recep Sade, Gokhan Polat, Mecit Kantarci “Unusual Cause of Seizure: Pott Puffy Tumor.” J Craniofac Surg, vol. 27, pp. 548-549, 2016. View at: Publisher Site | PubMed
- Samuel C Blackman, Mark R Schleiss “Forehead swelling caused by Pott's puffy tumor in a 9-year-old boy with sinusitis.” Pediatr Int, vol. 47, no. 6, 704-707, 2005. View at: Publisher Site | PubMed
- Sarah E Forgie, Thomas J Marrie “Pott's puffy tumor.” Am J Med, vol. 121, no. 12, pp. 1041-1042, 2008. View at: Publisher Site | PubMed
- N C Bambakidis, A R Cohen “Intracranial complications of frontal sinusitis in children: Pott's puffy tumor revisited.” Pediatr Neurosurg, vol. 35, no. 2, pp. 82-89, 2001. View at: Publisher Site | PubMed
- Michael Gupta, Hamdy El Hakim, Ravi Bhargava, et al. “Pott's puffy tumour in a pre-adolescent child: the youngest reported in the post-antibiotic era.” Int J Pediatr Otorhinolaryngol vol. 68, no. 3, pp. 373-378, 2004. View at: Publisher Site | PubMed
- Harbir Singh Arora, Nahed Abdel Haq “A 14-year-old male with swelling of the forehead. Pott’s puffy tumor.” Pediatric Ann, vol. 43, pp. 479-481. View at: Publisher Site | PubMed
- Phillip T Suwan, Suvarna Mogal, Subhash Chaudhary “Pott’s puffy tumor: an uncommon clinical entity.” Case Rep Pediatr, vol. 2012, 386104, 2012. View at: Publisher Site | PubMed
- Dimitris Kombogiorgas, Guirish A Solanki “The Pott puffy tumor revisited: neurosurgical implications of this unforgotten entity: case report and review of the literature.” J Neurosurg, vol. 105, no. 2, pp. 143-149, 2006. View at: Publisher Site | PubMed
